Table of Contents
What are the similarities and differences between intramembranous ossification and endochondral ossification?
Intramembranous ossification, as the name suggests, forms bone directly from sheets of mesenchymal connective tissue. This process is primarily responsible for creating flat bones like those found in your skull and clavicle. Picture it as a direct transformation – mesenchyme cells differentiate into osteoblasts, the bone-building cells, which lay down bone matrix.
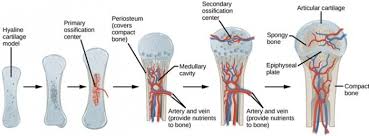
Endochondral ossification, on the other hand, uses a more indirect route. This process involves replacing a cartilage model with bone. You can think of it as a “scaffolding” method. Hyaline cartilage, a type of flexible connective tissue, serves as the initial framework. This process is responsible for creating most of your long bones, like those in your arms and legs.
The key difference between these two processes lies in the starting material. Intramembranous ossification begins with mesenchymal connective tissue, while endochondral ossification starts with hyaline cartilage.
Here’s a breakdown of the process of endochondral ossification, which will help you understand the growth of long bones:
1. Formation of a Cartilage Model: It all starts with a hyaline cartilage model. Think of this model as a mini version of the bone it will eventually become.
2. Growth of the Cartilage Model: The cartilage model grows in length through interstitial growth and in width through appositional growth.
Interstitial growth: This is a process where chondrocytes, the cartilage cells, divide and create new cartilage within the existing matrix.
Appositional growth: New cartilage is added to the surface of the existing cartilage.
3. Formation of the Bone Collar: A bone collar forms around the shaft of the cartilage model. This collar is formed by intramembranous ossification and is the first sign of bone formation.
4. Cavitation of the Cartilage Model: The cartilage in the center of the diaphysis (the shaft of the bone) begins to break down, creating spaces filled with blood vessels and cells from the perichondrium, the membrane surrounding the cartilage.
5. Invasion of the Cartilage Model by Blood Vessels and Osteoblasts: Blood vessels, along with osteoblasts, enter the spaces within the cartilage model. The osteoblasts begin to lay down bone matrix on the remnants of the cartilage.
6. Formation of the Primary Ossification Center: The region where the bone collar and the invading osteoblasts meet is called the primary ossification center. This center extends towards the ends of the bone.
7. Formation of the Secondary Ossification Center: Secondary ossification centers develop in the epiphyses (ends of the bones) during later stages of development. These centers are similar to the primary ossification center, but they occur at the ends of the bones.
8. Ossification of the Epiphyseal Plate: The epiphyseal plate, a region of hyaline cartilage that separates the diaphysis and epiphysis, allows for longitudinal growth of the bone. Eventually, the epiphyseal plate will be replaced by bone, resulting in the fusion of the diaphysis and epiphysis.
Growth plates, also known as epiphyseal plates, are crucial for the longitudinal growth of long bones. They are found between the diaphysis (shaft) and the epiphyses (ends) of long bones. These plates are made of hyaline cartilage and undergo continuous growth and replacement by bone throughout childhood and adolescence. The growth of these plates is regulated by hormones, including growth hormone and thyroid hormone, and plays a vital role in determining the final length of bones.
While intramembranous ossification directly forms bone from mesenchyme, endochondral ossification uses a more intricate process that involves replacing a cartilage model with bone. This process is key to the development and growth of most long bones in your body!
Which process is present in both intramembranous and endochondral ossification?
In intramembranous ossification, which forms flat bones like those in your skull, the bone collar acts as a protective barrier. It also helps to shape the developing bone and provides a point of attachment for the osteoblasts, the cells that create new bone tissue.
In endochondral ossification, which is responsible for forming most of your long bones like your femur, the bone collar serves a similar function. It protects the developing cartilage model, provides a point of attachment for osteoblasts, and helps to direct the growth of the bone.
The penetration of the diaphysis by a nutrient artery is actually a later stage in endochondral ossification. It occurs after the bone collar has formed and is critical for delivering nutrients to the growing bone tissue inside. However, it’s not a defining feature of both intramembranous and endochondral ossification.
Therefore, the presence of a bone collar during the early stages of bone development is a shared characteristic of both intramembranous and endochondral ossification. This collar is crucial for protecting and shaping the developing bone, and provides a base for the osteoblasts to begin creating new bone tissue.
Which of the following accurately compares endochondral ossification and intramembranous?
Endochondral ossification is like building a bone from a mold. It starts with a cartilage model that acts as a blueprint. This cartilage model is gradually replaced by bone tissue. Think of it like building a sandcastle with a mold. The sandcastle is the cartilage model, and the bone tissue is the hard, solid structure you build.
Intramembranous ossification, on the other hand, is a more direct process. Bone tissue forms directly within a membrane-like sheet of connective tissue. This method is like building a wall with bricks – you lay down the bricks directly, without a mold.
Here’s a table to help you visualize the differences:
| Feature | Endochondral Ossification | Intramembranous Ossification |
|——————|————————–|—————————–|
| Starting Point | Cartilage Model | Connective Tissue Membrane |
| Process | Replacement of Cartilage | Direct Bone Deposition |
| Examples | Long Bones | Flat Bones |
Endochondral ossification is responsible for creating most of our bones, especially the long bones like the femur and humerus. This process is how we grow taller! Intramembranous ossification is used to build the flat bones of the skull, the clavicle, and parts of the face.
To wrap it up, think of endochondral ossification as a gradual process where cartilage is replaced by bone, while intramembranous ossification is a more direct method of bone formation. Both processes are essential for building a strong and functional skeletal system.
What are the 2 types of ossification and what are there differences?
Intramembranous ossification is like building a house directly on the ground. It starts with a layer of mesenchyme, which is a type of connective tissue. This mesenchyme cells transform directly into bone cells, called osteoblasts. These osteoblasts create a framework of bone matrix, which is the material that makes up bone.
Endochondral ossification is more like building a house using a mold. In this process, a cartilage model is formed first. This cartilage model is like a template for the bone. Then, the cartilage is gradually replaced by bone.
So, intramembranous ossification is a direct process where bone is formed from mesenchyme, while endochondral ossification is an indirect process where bone is formed from a cartilage model.
Here’s a little more detail to help you understand the difference:
Intramembranous Ossification
Where it happens: This is how flat bones like the skull, clavicle, and parts of the face are formed.
Key players: Mesenchyme cells, which differentiate into osteoblasts, which produce bone matrix.
The process:
Mesenchyme cells cluster together and differentiate into osteoblasts.
Osteoblasts secrete bone matrix, which forms a network of bone.
Blood vessels grow into the bone, bringing nutrients and oxygen.
Bone matrix becomes mineralized, making the bone hard.
Endochondral Ossification
Where it happens: This is how most bones in the body are formed, including long bones like the femur and humerus.
Key players: Chondrocytes (cartilage cells), osteoblasts, osteoclasts (cells that break down bone).
The process:
Cartilage model forms.
Blood vessels invade the cartilage model, bringing in osteoblasts.
Osteoblasts start to replace the cartilage with bone, creating a bone collar around the outside of the model.
Chondrocytes in the center of the cartilage model die, leaving cavities.
Osteoblasts fill in these cavities with bone, creating the primary ossification center.
Secondary ossification centers form in the ends of the long bones.
Growth plates remain between the primary and secondary ossification centers, allowing for bone growth in length.
It’s important to note that both types of ossification are essential for the development of a healthy skeleton. Each process has its own unique role in creating the complex and intricate structure of bones.
What are the similarities and differences between a primary and a secondary ossification center?
Primary ossification centers are the first areas of bone formation in a developing bone. These centers form deep within the periosteal collar which is a layer of connective tissue surrounding the diaphysis, or shaft, of the bone. You’ll find them during endochondral ossification a process where cartilage is replaced by bone.
Secondary ossification centers also form through endochondral ossification, but they appear later in development. Unlike the single primary ossification center, secondary ossification centers are found in the epiphysis or ends of the bone. You’ll actually find two of these centers, one in each epiphysis.
Think of it like this: The primary ossification center is the foundation of the bone, forming the shaft, while the secondary ossification centers are like finishing touches, adding to the ends of the bone.
Let’s go a bit deeper:
The primary ossification center is where bone formation begins in the diaphysis. As the cartilage model grows, chondrocytes, the cells that make up cartilage, die and leave behind cavities. These cavities are invaded by blood vessels and osteoblasts, cells that produce bone. The osteoblasts start laying down bone matrix, replacing the cartilage and forming the diaphysis.
Secondary ossification centers emerge later in development, typically after birth. They form in the epiphyses, which are located at the ends of long bones. Just like in the diaphysis, the cartilage in the epiphyses is replaced by bone through endochondral ossification.
The key difference between the two is timing. The primary ossification center is the first to form, establishing the main shaft of the bone, while the secondary ossification centers appear later and add to the ends of the bone.
Why is this important? The epiphyseal plates, also known as growth plates, are located between the epiphysis and diaphysis and are responsible for lengthening the bone. These plates are made of cartilage and are only found in developing bones. Once the secondary ossification centers reach the epiphyseal plates, they merge, and the bone stops growing in length.
What are the similarities and differences between osteocytes osteoblasts and osteoclasts?
Osteoblasts are like construction workers, adding to the bone’s structure. They produce the protein collagen, which forms the framework of the bone, and they also release minerals like calcium and phosphate that harden the bone. Osteoclasts, on the other hand, are like demolition crews. They break down bone tissue, releasing minerals back into the bloodstream. This process, called bone resorption, is crucial for maintaining calcium levels in the blood and for repairing damaged bone.
Osteocytes are the most common type of bone cell, and they are embedded within the bone matrix. They act like sensors, detecting changes in pressure and strain on the bone. These signals help to direct the activity of osteoblasts and osteoclasts, ensuring that bone is deposited where it’s needed and removed where it’s not. For example, if a bone is subjected to a lot of stress, the osteocytes will send signals to osteoblasts to build more bone in that area. Conversely, if a bone is not being used much, the osteocytes will signal osteoclasts to remove bone, making it lighter and less dense.
So, you can think of osteoblasts, osteoclasts, and osteocytes as a team working together to maintain a strong and healthy skeleton. They are constantly working, building and breaking down bone, adapting to the body’s needs and ensuring that our bones are able to support us throughout our lives.
Is intramembranous ossification faster than endochondral ossification?
This study found that endochondral ossification often has a higher bone formation rate once a significant increase in bone formation is triggered. This is because endochondral ossification occurs at a faster pace (between 1 < S < 3) compared to intramembranous ossification. Think of it this way: endochondral ossification is like building a house from the ground up, with a sturdy foundation laid first. Intramembranous ossification, on the other hand, is more like a direct construction process, creating bone directly from mesenchymal cells. This "from the ground up" approach of endochondral ossification allows for faster bone formation. While the study suggests that endochondral ossification can have a higher formation rate, it's important to note that both types of ossification are vital for bone growth and development. Intramembranous ossification is responsible for forming flat bones like those in your skull and facial bones, while endochondral ossification forms long bones like your arms and legs. Both processes play crucial roles in our bodies, and understanding how they work helps us appreciate the complexity of bone formation.
What is the difference between intramembranous and endochondral ossification osmosis?
Intramembranous ossification is a direct process where mesenchymal tissue transforms directly into bone. This is how bones like the flat bones of the skull are formed. Imagine a sculptor shaping a clay model – that’s kind of what happens with intramembranous ossification.
On the other hand, endochondral ossification is a bit more indirect. Mesenchymal tissue first differentiates into cartilage, which acts like a temporary blueprint for the bone. This cartilage model is then gradually replaced by bone tissue. Think of it like building a sandcastle with a mold – the mold is the cartilage, and the sandcastle is the bone.
Here’s a more detailed explanation to help you visualize the process:
Intramembranous Ossification:
1. Mesenchymal Cells: The process starts with mesenchymal cells that are undifferentiated and have the potential to become various types of connective tissue.
2. Osteoblasts: These mesenchymal cells then differentiate into osteoblasts, which are the cells responsible for building bone.
3. Bone Matrix: The osteoblasts start secreting bone matrix, which is the organic and inorganic material that makes up bone tissue.
4. Ossification Centers: As the bone matrix is deposited, it forms ossification centers where bone tissue is formed. These centers gradually merge and grow until the entire bone is formed.
5. Blood Vessels: Blood vessels grow into the ossification centers, providing the necessary nutrients and oxygen for the process to continue.
Endochondral Ossification:
1. Mesenchymal Cells: Just like in intramembranous ossification, mesenchymal cells are the starting point.
2. Chondroblasts: However, in this case, the mesenchymal cells differentiate into chondroblasts, which are the cells that form cartilage.
3. Cartilage Model: The chondroblasts secrete cartilage matrix, forming a temporary cartilage model of the future bone. This model has the same shape as the future bone.
4. Calcification: As the cartilage model grows, the chondrocytes (mature cartilage cells) start to die. This triggers the calcification of the cartilage matrix, making it harder.
5. Bone Collar: A bone collar forms around the shaft of the cartilage model, which is the first sign of bone formation.
6. Blood Vessels: Blood vessels invade the calcified cartilage, bringing in osteoblasts and osteoclasts (cells that break down bone).
7. Bone Replacement: The osteoblasts begin replacing the calcified cartilage with bone tissue, forming the primary ossification center.
8. Secondary Ossification Centers: Secondary ossification centers develop in the ends of long bones, creating the epiphyses.
9. Epiphyseal Plate: A layer of cartilage, called the epiphyseal plate, remains between the epiphysis and diaphysis (shaft) of the bone. This plate allows for the continued growth of the bone until adulthood.
This difference in how bones are formed explains why different types of bones are formed via these two methods. Intramembranous ossification forms flat bones, while endochondral ossification forms long bones like those in your arms and legs.
What is the difference between intramembranous ossification and endochondral ossification quizlet?
Intramembranous ossification is a process where bone forms directly from mesenchymal tissue. Think of it as a sheet-like layer, which is why it’s often called “membrane bone formation.” It’s responsible for forming the flat bones of your skull, face, jaw, and the middle portion of your collarbone (clavicle).
Endochondral ossification, on the other hand, involves the replacement of cartilage with bone. It’s the primary process for forming most bones in your body, especially your long bones. This is the process that shapes your arms and legs, for example.
Here’s a deeper dive into each process:
Intramembranous Ossification
1. Mesenchymal cells cluster together and differentiate into osteoblasts, the cells responsible for creating new bone tissue.
2. These osteoblasts deposit a matrix of osteoid, which is the organic component of bone.
3. The osteoid then becomes mineralized, forming bone spicules, small, needle-like pieces of bone.
4. These bone spicules grow and fuse together to create a network of trabeculae (spongy bone).
5. Over time, the spaces between the trabeculae become filled with red marrow, which is responsible for blood cell production.
Endochondral Ossification
1. Hyaline cartilage forms a model of the future bone.
2. Chondrocytes, the cells that make up cartilage, begin to die off in the center of the model.
3. Blood vessels invade the area, bringing with them osteoblasts.
4. The osteoblasts deposit osteoid, replacing the dying cartilage with bone.
5. This process continues outwards, creating a primary ossification center.
6. As the bone grows longer, a secondary ossification center develops at the ends of the bone.
7. The epiphyseal plate, a layer of cartilage that remains between the primary and secondary ossification centers, allows for continued bone growth until adulthood.
Both intramembranous and endochondral ossification are fascinating processes that contribute to the formation of our skeletons. While they differ in their starting materials and methods, both ultimately result in the creation of strong and durable bone tissue.
See more new information: musicbykatie.com
Similarities Between Intramembranous And Endochondral Ossification: A Comparison
Okay, so you’re interested in intramembranous and endochondral ossification, huh? That’s cool! These are two major processes involved in bone formation in our bodies. They might seem different at first glance, but believe me, there are some pretty interesting similarities between them.
Let’s dive in and uncover these shared features, shall we?
A Foundation of Mesenchyme
Both intramembranous ossification and endochondral ossification begin with a special type of connective tissue called mesenchyme. This is the starting point for our bone journey. Mesenchymal cells have this cool ability to transform into different types of cells, making them the perfect building blocks for bone development.
Osteoblasts: The Bone Builders
One of the key similarities is the role of osteoblasts, the rockstar bone-building cells. They’re present in both intramembranous and endochondral ossification. These dedicated cells produce osteoid, the unmineralized bone matrix, which later becomes hardened by calcium deposition.
The Crucial Role of Vascularization
Both processes rely heavily on vascularization, meaning the formation of blood vessels. These blood vessels supply the necessary nutrients and oxygen for bone growth. Without them, our bones wouldn’t be able to thrive.
A Shared Final Product
At the end of the day, both intramembranous and endochondral ossification lead to the formation of lamellar bone. This is a highly organized structure composed of layers of bony tissue. Think of it as the finished product, the result of these complex processes.
Let’s Break Down the Similarities
Here’s a quick breakdown of the major similarities between these two bone formation processes:
Origin: Both start with mesenchyme.
Osteoblast Activity: Both involve osteoblasts producing osteoid, the precursor to bone.
Vascularization: Both require the formation of blood vessels to support growth.
Final Product: Both result in the formation of lamellar bone, the mature, organized bone tissue.
Intramembranous Ossification: The Direct Approach
Now, let’s talk about intramembranous ossification. This is a bit like a direct route. It involves the direct formation of bone from the mesenchyme without any intermediate cartilage formation. It’s the process responsible for forming flat bones like the skull, clavicle, and some parts of the face.
Here’s the breakdown:
1. Mesenchymal Cells Differentiate: Mesenchymal cells cluster together and differentiate into osteoblasts. These osteoblasts start secreting osteoid, the unmineralized bone matrix.
2. Osteoid Formation: Osteoid gets laid down in a haphazard way, forming spicules or small, needle-like structures.
3. Mineralization: As the osteoid is laid down, calcium salts deposit, hardening it into bone.
4. Trabecular Bone Formation: The spicules join together, forming a network of trabecular bone.
5. Periosteum Formation: A thin layer of connective tissue called the periosteum forms around the bone.
6. Bone Remodeling: The bone undergoes continuous remodeling, with osteoblasts adding new bone and osteoclasts removing old bone.
Endochondral Ossification: The Indirect Route
Endochondral ossification is a bit like the indirect route to bone formation. This process involves the formation of a cartilage model that serves as a temporary template for bone development. It’s the primary mechanism for forming long bones like those in our arms and legs, as well as the bones of the pelvis and vertebrae.
Here’s the breakdown:
1. Cartilage Model Formation: Mesenchymal cells differentiate into chondroblasts which form a cartilage model. This model is similar in shape to the final bone.
2. Perichondrium Formation: A layer of connective tissue called the perichondrium forms around the cartilage model.
3. Vascular Invasion: Blood vessels penetrate the perichondrium, bringing in osteoblasts.
4. Bone Collar Formation: Osteoblasts in the perichondrium deposit osteoid, forming a bone collar around the cartilage model.
5. Cartilage Degradation: As the cartilage model grows, it starts to break down.
6. Ossification Center: Osteoblasts invade the degenerating cartilage, laying down osteoid and forming a primary ossification center.
7. Secondary Ossification Center: Secondary ossification centers form in the epiphyses (ends of the long bones) later on.
8. Epiphyseal Plate: A layer of cartilage called the epiphyseal plate remains between the epiphysis and the diaphysis (shaft of the bone). This plate is responsible for longitudinal growth.
9. Bone Remodeling: Throughout life, bone remodeling continues, with osteoblasts and osteoclasts working together to maintain bone structure.
Similarities in Action: A Look at Bone Remodeling
Both intramembranous and endochondral ossification are not one-time events. They’re followed by a continuous process called bone remodeling. This ongoing process ensures that our bones stay strong, adapt to stress, and repair injuries.
Bone remodeling involves the coordinated activity of osteoblasts and osteoclasts. Osteoblasts add new bone while osteoclasts break down old bone. This constant turnover is essential for maintaining bone health, strength, and flexibility.
Understanding the Importance
Knowing about these bone formation processes is super important for many reasons. They give us a better understanding of how our bodies develop and grow. Understanding how bones are formed helps us to understand bone diseases like osteoporosis. It also helps doctors treat bone fractures and other injuries more effectively.
FAQs
What are the main differences between intramembranous and endochondral ossification?
Intramembranous ossification forms bone directly from mesenchyme, while endochondral ossification uses a cartilage template. Intramembranous ossification is involved in forming flat bones, while endochondral ossification forms long bones.
Is it possible to have both processes happening at the same time?
Yes, both intramembranous and endochondral ossification can occur at the same time during development. For example, the formation of the skull involves both processes.
How does bone remodeling play a role in bone repair?
Bone remodeling is crucial for bone repair. When a bone breaks, osteoclasts remove the damaged bone, and osteoblasts lay down new bone, filling in the gap and restoring the structure.
Are there any diseases that affect these processes?
Yes, there are several diseases that can affect bone formation, including osteogenesis imperfecta (brittle bone disease), achondroplasia (dwarfism), and osteoporosis.
What are some things I can do to maintain bone health?
To keep your bones strong, it’s important to have a healthy diet rich in calcium and vitamin D. Regular exercise, especially weight-bearing activities, also helps strengthen bones.
So, there you have it! The fascinating similarities between intramembranous and endochondral ossification. Now you know about the direct and indirect routes to bone formation, the shared players like osteoblasts and vascularization, and the constant remodeling that keeps our bones healthy. Remember, understanding these processes helps us appreciate the complexity of our bodies and how they work.
6.4 Bone Formation and Development – Anatomy
In intramembranous ossification, bone develops directly from sheets of mesenchymal connective tissue, but in endochondral ossification, bone develops by replacing hyaline cartilage. Open Educational Resources
Making and shaping endochondral and intramembranous bones
In bony vertebrates, bones primarily develop in two ways via endochondral or intramembranous bone differentiation. In endochondral bones, ossification occurs within the cartilaginous template and also within the surrounding fibroblastic perichondral National Center for Biotechnology Information
Endochondral ossification: Anatomy and histology | Kenhub
Endochondral ossification is one of the two ways by which bone is formed. The process of bone formation and development begins as an embryo and continues until early adulthood. Endochondral ossification occurs in the long bones around the 6th Kenhub
Intramembranous & Endochondral Ossification | Difference
There are two types of bone growth: intramembranous and endochondral ossification. Intramembranous ossification is the formation of bones specifically in the skull as well as the clavicles… Study.com
Mechanisms of bone development and repair – Nature
Bone formation during embryogenesis occurs in two distinct processes: intramembranous ossification or endochondral ossification. Intramembranous ossification begins with the condensation… Nature
5.4: Bone Formation and Development – Medicine
Q. In what ways do intramembranous and endochondral ossification differ? Answer. A. In intramembranous ossification, bone develops directly from sheets of mesenchymal connective tissue, but in Medicine LibreTexts
Bone formation: Histology and process of the ossification
Intramembranous ossification is characterized by the formation of bone tissue directly from mesenchyme. Flat bones, such as the parietal and occipital bones, are formed using this process. On the contrary, endochondral ossification is dependent on a Kenhub
Embryology, Bone Ossification – StatPearls – NCBI
Intramembranous ossification directly converts the mesenchymal tissue to bone and forms the flat bones of the skull, clavicle, and most of the cranial bones. National Center for Biotechnology Information
Intramembranous ossification and endochondral
Osteoporosis impairs fracture healing and prognosis, but how intramembranous ossification (IO) or endochondral ossification (EO) during fracture healing are affected and whether these two… Nature
Intramembranous And Endochondral Ossification
Intramembranous Vs Intracartilagenous Ossification 🦴 | Anatomy Series
Osteogenesis (Bone Formation): Intramembranous Ossification – Physiology | Lecturio Nursing
Intramembranous Ossification
Ossification | Bone Formation | Histogenesis Of Bone | Bone Histology | Embryology Of The Skeleton
Endochondral And Intramembranous Bone Formation
6. Ossification
Intramembranous And Endochondral Ossification
Link to this article: similarities between intramembranous and endochondral ossification.
See more articles in the same category here: https://musicbykatie.com/wiki-how/
