Table of Contents
How do you test for choledocholithiasis?
Abdominal CT scans are an excellent tool to see if stones are present, as they provide detailed images of your bile duct. Abdominal ultrasounds are another valuable tool to detect these stones, especially if they are located closer to the gallbladder.
Finally, endoscopic retrograde cholangiopancreatography (ERCP) is a more invasive procedure but offers the most precise view of the bile duct and can even remove the stones during the same procedure.
Let’s delve a bit deeper into each of these tests:
Abdominal CT Scan: This test uses X-rays to create detailed cross-sectional images of your abdomen, highlighting any abnormalities like stones in your bile duct. This test is fast and painless, usually taking less than 30 minutes to complete.
Abdominal Ultrasound: This non-invasive test uses sound waves to create images of your internal organs, including your bile duct. It is a painless procedure that is often used as a first-line test for diagnosing choledocholithiasis.
Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure involves passing a thin, flexible tube (endoscope) with a tiny camera attached through your mouth, down your esophagus, and into your bile duct. A special dye is then injected into the bile duct, allowing doctors to view its structure and any stones present on a screen. The same procedure can also be used to remove the stones if they are found.
Choosing the best test for you depends on various factors, including the suspected location of the stones, the severity of your symptoms, and your overall health status. Your doctor will advise on the most suitable test based on your individual situation.
What tests are performed to identify the presence of melena?
The digital rectal examination is a simple procedure where a doctor inserts a gloved finger into the rectum to feel for any abnormalities. This can help determine the source of the melena, as blood from the lower gastrointestinal tract may be visible in the rectum. However, it is important to note that a digital rectal examination alone cannot definitively diagnose melena.
In addition to a digital rectal examination, other tests may be used to confirm melena. These tests include:
Stool guaiac test: This test checks for the presence of blood in the stool.
Colonoscopy: This procedure involves inserting a flexible tube with a camera attached into the colon to visualize the lining of the colon.
Endoscopy: This procedure involves inserting a thin, flexible tube with a camera attached into the esophagus, stomach, and duodenum to visualize the lining of these organs.
It is crucial to note that melena can be a serious medical condition, and it is essential to seek medical attention if you experience black, tarry stools. The presence of melena often suggests bleeding in the upper gastrointestinal tract, which may be caused by various conditions, including ulcers, gastritis, and cancer. Early diagnosis and treatment are critical for managing melena and preventing complications.
What test would most likely detect an ulcer?
The endoscope can also be used to take biopsies of any suspicious areas. These biopsies can then be examined under a microscope to confirm the presence of an ulcer and determine its cause. The doctor may also look for signs of inflammation, infection, or other conditions that may be contributing to your symptoms. An upper GI endoscopy is a safe and effective procedure that can provide valuable information about your digestive health.
What is the medical term for bursting forth of blood from the spleen?
Splenorrhexis is a rare condition that can be caused by a number of factors, including trauma, infections, and certain diseases. The spleen is a vital organ that filters blood and helps to fight infections. When the spleen ruptures, it can lead to a significant amount of internal bleeding.
Symptoms of splenorrhexis include:
Abdominal pain
Tenderness in the left upper abdomen
Weakness
Dizziness
Shock
Rapid heart rate
Low blood pressure
If you experience any of these symptoms, it is important to seek medical attention immediately.
Treatment for splenorrhexis usually involves surgery to repair the ruptured spleen. In some cases, it may be necessary to remove the spleen entirely. After surgery, it is important to follow your doctor’s instructions carefully to ensure that you recover fully.
Which test would demonstrate choledocholithiasis medical term?
Doctors use advanced imaging to definitively diagnose choledocholithiasis. These tests allow them to visualize the bile ducts and see if there are any stones present. Here are the most common imaging tests used:
Magnetic Resonance Cholangiopancreatography (MRCP): This is a non-invasive test that uses magnetic fields and radio waves to create detailed images of the bile ducts. It’s a good first-line test because it’s painless and doesn’t involve any radiation.
Endoscopic Retrograde Cholangiopancreatography (ERCP): ERCP is a minimally invasive procedure where a thin, flexible tube (endoscope) is inserted through the mouth and into the small intestine. A dye is then injected into the bile ducts, allowing them to be visualized on an X-ray. This test is often used to both diagnose and treat choledocholithiasis because it allows the doctor to remove the stones directly.
Endoscopic Ultrasound (EUS): Similar to ERCP, EUS involves inserting an endoscope through the mouth. However, EUS uses sound waves to create detailed images of the bile ducts. This test is particularly helpful for visualizing small stones that may be missed by other imaging techniques.
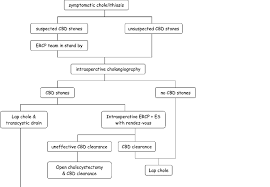
Intraoperative Cholangiography (IOC): IOC is a test that is performed during surgery. Dye is injected into the bile ducts, allowing them to be visualized on an X-ray. This is a valuable tool for detecting choledocholithiasis during surgery.
Intraoperative Ultrasound (IUS): This test uses ultrasound waves to create images of the bile ducts during surgery. It can be helpful in identifying stones and planning the surgical approach.
Let’s dive a little deeper into ERCP, since it’s often the gold standard for diagnosing and treating choledocholithiasis. ERCP is a minimally invasive procedure that’s performed by a gastroenterologist. It’s usually done as an outpatient procedure, meaning you’ll be able to go home the same day.
Here’s a breakdown of how it works:
1. Preparation: Before the procedure, you’ll be given medication to help you relax and to numb your throat. You may also need to fast for a few hours before the procedure.
2. Insertion: The doctor will insert a thin, flexible tube called an endoscope through your mouth and into your small intestine. The endoscope has a camera attached to it, which allows the doctor to see inside your digestive tract.
3. Dye Injection: Once the endoscope is in place, the doctor will inject a special dye into the bile ducts. This dye helps the bile ducts show up clearly on an X-ray.
4. X-Ray Images: The doctor will then take X-ray images of the bile ducts. These images will reveal the presence or absence of stones.
5. Stone Removal: If stones are found, the doctor can often remove them during the same procedure. They will use a specialized tool to grab and remove the stones from the bile ducts.
ERCP is a safe and effective procedure, but like any medical procedure, there are potential risks. These risks include bleeding, infection, and pancreatitis. Your doctor will discuss the risks and benefits of ERCP with you before the procedure.
What is the best diagnostic tool for choledocholithiasis?
Let’s break down why endoscopic ultrasonography shines when it comes to diagnosing choledocholithiasis.
Endoscopic ultrasonography combines the power of endoscopy and ultrasound. Endoscopy allows a flexible, thin tube with a camera attached to it to be inserted into the digestive tract. This gives doctors a direct view of the inside of the bile duct. Ultrasound waves are then used to create detailed images of the bile duct and surrounding tissues. This combination provides a highly detailed picture of the bile duct, making it easier to detect even small stones.
Other diagnostic tools, like abdominal ultrasound, magnetic resonance cholangiopancreatography (MRCP), and computed tomography (CT) scans, can also be used to diagnose choledocholithiasis. However, endoscopic ultrasonography is preferred because it offers a higher level of accuracy, especially for detecting smaller stones. Additionally, endoscopic ultrasonography can be used not only for diagnosis but also for treatment. During the same procedure, doctors can use special instruments to remove the stones from the bile duct. This makes it a very effective tool for managing choledocholithiasis.
What lab test for melena?
The fecal occult blood test is a simple and non-invasive test. It involves collecting a small sample of your stool and applying a chemical reagent to it. If blood is present in the stool, the reagent will cause a color change.
This test can be done in a doctor’s office, a clinic, or at home. If the test is positive, it means that there is blood in your stool, but it doesn’t tell your doctor where the bleeding is coming from.
To diagnose the cause of your bleeding, your doctor may order additional tests, such as an endoscopy, which is a procedure that allows your doctor to look inside your digestive tract. An endoscopy can help your doctor identify the source of bleeding and determine the best treatment.
Remember, melena is a serious condition, but it can be treated effectively with the right diagnosis and treatment.
How do you assess for melena?
To find out, your doctor will likely do an upper endoscopy first. This is a procedure where they use a thin, flexible tube with a camera on the end to look inside your esophagus, stomach, and duodenum. If the upper endoscopy doesn’t show any bleeding, then they might do a colonoscopy to look for a source of bleeding in your colon.
A colonoscopy is a procedure where a thin, flexible tube with a camera on the end is inserted into the rectum to examine the lining of the colon. It’s a safe and common procedure, and it can help doctors find the source of bleeding and determine the best course of treatment.
It’s important to remember that melena can be a symptom of serious medical conditions, so if you’re experiencing it, it’s important to see your doctor right away.
The upper endoscopy is the first step in diagnosing melena because it can identify a wide range of causes of upper gastrointestinal bleeding, including ulcers, gastritis, and tumors. If the upper endoscopy is negative, the colonoscopy can help identify bleeding sources in the colon.
These procedures are both important tools in diagnosing melena and finding the source of the bleeding.
How can you tell the difference between melena and iron stool?
Melena is black, tarry stool caused by digested blood in the digestive tract. To help someone understand what melena looks like, you can compare it to black asphalt or a very dark, almost black, piece of chocolate or even a black tarpaulin. Melena can also be sticky, which is something people often remember.
Iron supplements can also darken stool color, but it’s usually a less intense black, often described as dark green or very dark brown. It may also have a more “muddy” consistency, unlike the stickiness of melena.
If you’re unsure, it’s always best to consult with a doctor. They can help determine the cause of the dark stool and recommend the appropriate course of action.
Here are some other things to consider when trying to differentiate melena from a stool darkened by iron:
Amount of blood:Melena often indicates significant bleeding in the upper gastrointestinal tract, so the stool might be very dark and have a strong odor.
Symptoms: Other symptoms associated with melena might include abdominal pain, vomiting blood, or weakness.
Iron dosage: The amount of iron supplement taken can affect the stool’s color. Higher doses can lead to a more intense black color.
Remember, while iron supplements can cause dark stools, melena is a more serious condition that requires prompt medical attention.
Can a blood test detect a bleeding ulcer?
It’s important to understand how these blood tests work. The FBC measures different types of blood cells, including red blood cells. If you have a bleeding ulcer, you might have fewer red blood cells than usual, which indicates anemia. This is because your body is losing blood due to the ulcer.
In addition to the FBC, your doctor might also order kidney function blood tests, especially if your ulcer was caused by using NSAID medications. These medications can sometimes affect your kidneys, so it’s important to monitor them closely.
Remember, these blood tests are just one tool to help your doctor assess your health and understand what’s going on with your body. If you have any concerns about your health, don’t hesitate to talk to your doctor. They can guide you through the right tests and treatments to get you back on the road to recovery.
See more here: What Tests Are Performed To Identify The Presence Of Melena? | What Test Would Demonstrate Choledocholithiasis
How is choledocholithiasis diagnosed?
First off, they’ll probably check your blood. High levels of bilirubin and liver enzymes can be a tip-off that something’s amiss in your bile duct. This is because those gallstones can block the flow of bile, causing a backup.
Next up, they’ll usually do an ultrasound. This painless test uses sound waves to create images of your insides. They’re looking for a dilated common bile duct (which means it’s wider than it should be) and a shadow that could indicate a gallstone.
But here’s the thing: sometimes, even with an ultrasound, those pesky gallstones can be sneaky and hide! That’s why doctors might use a more advanced imaging technique called an endoscopic retrograde cholangiopancreatography (ERCP). This procedure allows your doctor to get a really good look at your bile duct and pancreas by inserting a thin, flexible tube with a camera on the end into your mouth and down your digestive system. It’s like giving your doctor a virtual tour of your bile duct!
During an ERCP, your doctor can also take biopsies, if needed, to confirm the diagnosis and to see if there’s any inflammation. They can even remove the gallstone using a special tool inserted through the scope.
So, if you’re worried about choledocholithiasis, don’t hesitate to talk to your doctor. They can guide you through the right tests and treatments to get you feeling better.
What are the preoperative tests for choledocholithiasis?
The standard tests doctors use to evaluate you for choledocholithiasis are liver function tests and an abdominal ultrasound. These tests, combined with your medical history and physical exam, are usually enough to figure things out. If there’s something unusual in the results, it could mean you have choledocholithiasis.
Liver function tests (LFTs) are a group of blood tests that measure how well your liver is working. The liver is responsible for many important functions, including filtering waste products from the blood, producing bile, and regulating blood sugar. If there are problems with your liver, it can affect the flow of bile, which could be a sign of choledocholithiasis.
An abdominal ultrasound uses sound waves to create images of the inside of your abdomen. This test can help doctors visualize your gallbladder, bile ducts, and other organs in the area. If there are any stones in your bile ducts, the ultrasound will likely pick them up.
It’s important to note that these tests are usually just the starting point. Depending on the results, your doctor might recommend other tests, like magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP).
These tests are important for planning your treatment. Choledocholithiasis can lead to serious complications like cholangitis (infection of the bile ducts) and pancreatitis (inflammation of the pancreas). Early detection and treatment are crucial for preventing these problems.
Can ultrasound confirm choledocholithiasis?
While a normal liver function test (LFT) and a transabdominal ultrasound of the right upper quadrant (RUQ) can help rule out choledocholithiasis, they’re not always reliable for making a definitive diagnosis. CBD stones (stones in the common bile duct) are often difficult to see on ultrasound. This is because ultrasound waves can be affected by things like gas in the intestines, making it hard to get a clear picture of the bile duct.
For patients over 55, the chance of having choledocholithiasis is also lower. This is because the condition is more common in younger individuals.
So, what does this mean? It means that ultrasound might not be enough to confirm choledocholithiasis, even if your LFTs are normal and the ultrasound doesn’t show any obvious signs of stones. To be completely sure, your doctor will likely recommend additional tests, such as:
Endoscopic retrograde cholangiopancreatography (ERCP): This is a procedure where a thin, flexible tube with a camera on the end is inserted through your mouth into your digestive system. This allows your doctor to directly visualize the bile duct and look for stones.
Magnetic resonance cholangiopancreatography (MRCP): This is a non-invasive imaging test that uses magnetic fields and radio waves to create detailed images of the bile duct.
Remember: If you have any symptoms of choledocholithiasis, such as abdominal pain, jaundice, or fever, it’s important to see your doctor for a proper diagnosis and treatment plan. They’ll be able to guide you through the best course of action based on your individual situation.
What is choledocholithiasis?
Gallstones are small, hard deposits that form in your gallbladder. They’re usually made of cholesterol and can vary in size. The gallbladder is a small, pear-shaped organ that stores bile, a fluid that helps digest fats. Bile travels from the gallbladder through the common bile duct and into the small intestine.
When gallstones form in the gallbladder, they can sometimes pass through the common bile duct. If they get stuck, they can block the flow of bile, leading to choledocholithiasis.
Symptoms of choledocholithiasis can vary depending on the size and location of the gallstones. Some people may not have any symptoms at all, while others may experience pain, jaundice, fever, and chills.
If you’re experiencing any of these symptoms, it’s important to see a doctor to get a diagnosis. Early diagnosis and treatment can help prevent serious complications.
See more new information: musicbykatie.com
What Test Would Demonstrate Choledocholithiasis: A Guide
Choledocholithiasis is a fancy way of saying that you have stones in your common bile duct, which is the tube that carries bile from your liver to your small intestine. These stones can cause a whole lot of trouble, from pain to jaundice, and sometimes even infection.
So how do we figure out if you have choledocholithiasis? We have a few tricks up our sleeves.
Tests that can demonstrate choledocholithiasis:
1. Ultrasound:
* This is a great starting point, kind of like the basic checkup. It uses sound waves to create images of your liver, gallbladder, and bile ducts.
* If we see a stone hanging out in your common bile duct, bingo!
Ultrasound is painless and pretty quick, so it’s our go-to test.
Ultrasound is a good test for gallstones because it is non-invasive and can be done relatively quickly.
Ultrasound uses sound waves to create images of your liver, gallbladder, and bile ducts, and it can often detect stones in these areas.
Ultrasound can also identify dilatation of the common bile duct, which is a sign that there may be a stone obstructing the flow of bile.
Ultrasound is a non-invasive imaging study that uses sound waves to create images of internal organs and tissues.
Ultrasound is a non-invasive imaging technique that utilizes sound waves to create images of internal organs.
Ultrasound is a non-invasive, painless test that can be done in an outpatient setting.
Ultrasound is a valuable tool for diagnosing choledocholithiasis, but it is not always perfect.
2. Endoscopic retrograde cholangiopancreatography (ERCP):
* This one’s a little more involved.
* It’s basically a fancy camera attached to a thin, flexible tube that goes down your throat and into your small intestine.
* We can use a dye to highlight the bile duct, making it easier to spot any stones.
* But wait, there’s more! We can actually remove those stones with the ERCP, which is a pretty neat trick.
ERCP is a diagnostic and therapeutic procedure that allows us to visualize the bile duct and pancreatic duct, and to remove any stones that may be present.
ERCP is a sensitive and specific test for choledocholithiasis.
ERCP is a minimally invasive procedure that can be performed under sedation.
ERCP is a good option for diagnosing choledocholithiasis if other tests are inconclusive, or if the patient is experiencing symptoms that suggest a stone is blocking the bile duct.
ERCP is a specialized procedure that is typically performed by a gastroenterologist.
ERCP is a good test to use when there is suspicion of choledocholithiasis as it can both diagnose and treat the condition.
3. Magnetic resonance cholangiopancreatography (MRCP):
* This test uses a magnetic field and radio waves to create detailed images of your bile ducts.
MRCP is great for picking up those little stones that might be hiding.
MRCP is a non-invasive test that does not require any contrast.
MRCP can be helpful if you’re not a good candidate for ERCP, or if we want to avoid the risks of a more invasive procedure.
MRCP is a safe and effective test that is often used as an alternative to ERCP for diagnosing choledocholithiasis.
MRCP can be performed in a hospital or outpatient imaging center.
4. Hepatobiliary scintigraphy:
* This test uses a radioactive tracer to track the flow of bile from your liver to your small intestine.
* If there’s a stone in your common bile duct, the bile will get stuck, and the scan will show it.
Hepatobiliary scintigraphy is a sensitive test for choledocholithiasis, but it is not as specific as ERCP or MRCP.
Hepatobiliary scintigraphy is a good option for diagnosing choledocholithiasis if other tests are inconclusive.
Choosing the right test:
* So which test is right for you?
Ultrasound is usually the first test we’ll do, because it’s easy and affordable.
* If ultrasound isn’t enough to tell the whole story, we might move on to ERCP, MRCP, or hepatobiliary scintigraphy.
* Your doctor will help you decide what’s best based on your symptoms, your medical history, and your individual situation.
FAQs about Choledocholithiasis:
What are the symptoms of choledocholithiasis?
Pain: You might feel pain in your upper abdomen, which can spread to your back.
Jaundice: This is a yellowing of your skin and whites of your eyes. It happens because the bile can’t get to your small intestine to help you digest fats.
Fever: This can be a sign of infection in your bile ducts.
Chills: You might also experience chills, especially if you have an infection.
Nausea and vomiting: You might feel sick to your stomach and vomit.
Diarrhea or constipation: Your bowel habits might change.
Light-colored stools: If the bile is blocked, your stools might appear pale.
Dark urine: Your urine might be darker than usual.
What causes choledocholithiasis?
* It’s usually caused by gallstones that travel from your gallbladder to your common bile duct.
* Sometimes stones can form directly in the common bile duct, but this is less common.
Choledocholithiasis can happen to anyone, but it’s more common in people who are overweight, have high cholesterol, or have a family history of gallstones.
What is the treatment for choledocholithiasis?
Treatment depends on the size and location of the stone and your overall health.
If the stone is small, it might pass on its own with a little help from medications.
If the stone is larger, we might need to remove it.
ERCP is often used to remove stones, but surgery may be needed in some cases.
Treatment for choledocholithiasis is usually successful, but it’s important to see a doctor if you have any symptoms.
What can I do to prevent choledocholithiasis?
* There’s no guaranteed way to prevent choledocholithiasis, but here are some things that might help:
Maintain a healthy weight: Being overweight increases your risk of developing gallstones, which can lead to choledocholithiasis.
Eat a healthy diet: A diet low in fat and cholesterol might help prevent gallstones.
Exercise regularly: Getting regular exercise can help you maintain a healthy weight and reduce your risk of gallstones.
Talk to your doctor: If you have a family history of gallstones, talk to your doctor about your risk factors and what you can do to prevent them.
Are there any long-term complications from choledocholithiasis?
* If left untreated, choledocholithiasis can lead to serious complications, such as:
Infections: A blocked bile duct can lead to infection in the bile duct or liver.
Pancreatitis: This is inflammation of the pancreas, which can be caused by a stone blocking the pancreatic duct.
Cirrhosis: This is scarring of the liver, which can happen if the bile duct is blocked for a long time.
Liver failure: This is a rare but serious complication that can occur if the bile duct is blocked and the liver is damaged.
Choledocholithiasis can be a tricky condition, but with the right tests and treatment, it’s usually manageable. If you’re experiencing symptoms, don’t hesitate to see a doctor. We’ll work together to figure out the best course of action for you.
Choledocholithiasis: What Is It, Causes, Diagnosis,
To demonstrate choledocholithiasis, blood tests can be done to look for high levels of bilirubin and liver enzymes. Initially, a transabdominal ultrasound can be performed to look for dilation of the Osmosis
Choledocholithiasis: Evaluation, Treatment, and Outcomes
The diagnosis of choledocholithiasis is initially suggested by symptomatology, laboratory tests, and ultrasound (US) findings. National Center for Biotechnology Information
Choledocholithiasis and Cholangitis – Hepatic and Biliary
Key Points. Choledocholithiasis is the presence of stones in bile ducts; the stones can form in the gallbladder or in the ducts themselves. These stones cause biliary colic, MDS Manuals
Choledocholithiasis: Clinical manifestations, diagnosis, and
This topic will review the clinical manifestations and diagnosis of choledocholithiasis. The treatment of choledocholithiasis, as well as the epidemiology UpToDate
Choledocholithiasis: Causes, Symptoms, and Diagnosis
If you have symptoms, a doctor will want to verify the presence of a gallstone in the common bile duct. He or she may use one of the following imaging tests: Healthline
Choledocholithiasis: Evolving standards for diagnosis and
The standard preoperative workup for patients presenting with symptoms attributable to cholelithiasis includes liver function tests, and abdominal ultrasound. National Center for Biotechnology Information
Choledocholithiasis – Gastrointestinal – Medbullets
Physical exam reveals tenderness to palpation in the right upper quadrant and negative Murphy sign. Laboratory results show increased alkaline phosphatase and total bilirubin. A right upper Medbullets
Choledocholithiasis – Knowledge @ AMBOSS
Choledocholithiasis refers to the presence of gallstones in the common bile duct (CBD). Characteristic clinical features include right upper quadrant pain and signs AMBOSS
Choledocholithiasis Information | Mount Sinai – New York
You may also have blood tests to check your liver function and to see if your bilirubin levels are too high. You may not need to treat gallstones, unless they’re causing symptoms. If that’s the case, your doctor will Mount Sinai Health System
Gallbladder: Cholelithiasis Vs Cholecystitis Vs Choledocholithiasis Vs Cholangitis [Made Easy]
Cholelithiasis Associated With Choledocholithiasis.
Murphy Sign – Clinical Examination
Pre-Op Evaluation: Identifying Patients At Risk And Making The Diagnosis
Ercp (Endoscopic Retrograde Cholangiopancreatography) -Procedure 3D Animation
Cholecystitis Vs Cholelithiasis Vs Cholangitis Vs Choledocholithiasis [Nursing, Usmle]
Is It Possible To Have Gallbladder Symptoms Without Gallstones?
Scanning Technique: Gallbladder
Link to this article: what test would demonstrate choledocholithiasis.
See more articles in the same category here: https://musicbykatie.com/wiki-how/
