Table of Contents
What are pneumatized mastoid air cells?
The pneumatization process depends on a few factors, such as the person’s overall health and the shape of their mastoid bone. These factors influence how many air cells develop, their size, and how they are arranged. Think of it like this: A person’s mastoid bone is a blueprint, and pneumatization is the building process, resulting in a unique structure for each person.
Pneumatization is important because it helps to lighten the skull, and it also helps to protect the middle ear. The air cells act as a buffer, absorbing sound waves and preventing them from damaging the delicate structures of the ear. Pneumatization also helps to drain fluid from the middle ear, which is important for keeping the ear healthy.
If you’re curious about pneumatized mastoid air cells or have any concerns about your hearing, talk to your doctor. They can give you more information about this process and how it affects your health.
What is the theory of Pneumatization of the mastoid?
There are a few different theories about how the mastoid process, the bony part behind your ear, gets filled with air. One of the most well-known theories is Wittmaack’s endodermal theory, which was proposed in 1918.
Wittmaack’s theory suggests that a healthy middle ear lining, called the mucosa, is key for normal pneumatization. This means that if the middle ear gets inflamed, or if the Eustachian tube (the passage connecting the middle ear to the back of your nose) isn’t working properly, it can hinder the process of the mastoid becoming filled with air.
Think of it like this: The middle ear is like a small room, and the mastoid is like an adjoining storage space. Normally, air travels through the Eustachian tube from the nose and into the middle ear. This air pressure helps keep the middle ear healthy. If the Eustachian tube is blocked, air can’t get in, and the middle ear can become stuffy.
According to Wittmaack, if the middle ear lining is irritated or inflamed, it can also interfere with the normal air flow into the mastoid process. This means that the mastoid won’t get as much air as it should, and it might not develop properly.
It’s important to remember, though, that Wittmaack’s theory isn’t the only explanation for how the mastoid gets filled with air. There are other theories out there, and more research is always being done to understand this process fully.
What are the types of mastoid Pneumatization radiology?
Pneumatic mastoids are fully developed, meaning they’re filled with air cells. These cells are connected to the middle ear and help to regulate pressure within the ear. Sclerotic mastoids, on the other hand, are solid bone and lack air cells. This can be due to various factors, including genetics or chronic ear infections. Diploic mastoids have bone marrow instead of air cells. Finally, mixed mastoids exhibit a combination of air cells and bone marrow.
Understanding the different types of mastoid pneumatization is crucial in radiology for several reasons. First, it helps radiologists assess the health of the mastoid bone. For instance, a sclerotic mastoid might indicate a history of ear infections, while a pneumatic mastoid suggests a healthy mastoid bone. Second, it helps radiologists differentiate between normal anatomical variations and pathological conditions, such as cholesteatoma.
Let’s delve a bit deeper into each type:
Pneumatic: A pneumatic mastoid is considered the most common type. It’s characterized by a large number of air cells that are interconnected and extend throughout the mastoid process. This type is usually associated with a healthy middle ear.
Sclerotic: In contrast, a sclerotic mastoid lacks air cells and is dense with bone. This type is often seen in patients who have had recurrent ear infections or chronic otitis media. The density of the bone can make it difficult to visualize the structures within the mastoid on imaging.
Diploic: A diploic mastoid is filled with bone marrow, rather than air cells. This type is less common than the other types and is often associated with a smaller mastoid process.
Mixed: A mixed mastoid displays a combination of air cells and bone marrow. It’s considered a transitional type, meaning it can evolve over time. For example, a pneumatic mastoid can become mixed as a result of aging or chronic ear infections.
The type of mastoid pneumatization can have implications for surgical procedures. For example, if a patient has a sclerotic mastoid, the surgeon might need to use different techniques to access the middle ear.
By understanding the different types of mastoid pneumatization, radiologists can better interpret imaging studies and provide clinicians with valuable information for patient care.
At what age are mastoid air cells aerated?
This means that the mastoid bone, located behind the ear, has developed a system of interconnected air spaces. These air cells are connected to the middle ear and help to regulate pressure and drain fluids. The development of these air cells is an important part of healthy ear function.
Pneumatization is a complex process that involves the growth of bone and the formation of air spaces. It’s influenced by several factors, including genetics and environmental factors. The process can vary in speed and extent from person to person. However, by the age of six, most children have fully developed mastoid air cells.
While the mastoid is usually fully pneumatized by age six, it’s important to remember that this is a general guideline. Some individuals may develop fully pneumatized mastoid bones earlier or later than this. Additionally, the size and shape of mastoid air cells can vary significantly between individuals.
The development of mastoid air cells is essential for proper ear function. They contribute to sound transmission, pressure regulation, and fluid drainage. If the pneumatization process is delayed or incomplete, it can increase the risk of ear infections and other ear problems.
What is the meaning of Pneumatization?
Think of it like this: imagine a hollow plastic container. It’s much lighter than a solid block of plastic, right? The same principle applies to bones. Pneumatization allows bones to be sturdy and strong, but without the heavy weight of solid bone. This is especially important for bones in the head, where a lightweight structure is crucial for mobility.
Let’s break down pneumatization further. These air-filled cavities are not just empty spaces. They’re lined with a thin layer of tissue called mucosa, which helps to keep the cavities clean and free of infection. The mucosa also produces a special fluid that helps to lubricate the bones and prevent them from rubbing together.
Pneumatization is a complex process that starts during fetal development. As the fetus grows, the bones begin to develop these air-filled spaces through a process called bone remodeling. This process involves the breakdown of old bone tissue and the creation of new bone tissue. In the case of pneumatization, the breakdown of bone tissue creates the air-filled cavities.
The extent of pneumatization can vary from person to person, and it can also be affected by factors such as age and health. For example, pneumatization is more common in adults than in children. It can also be affected by conditions like sinusitis, which can cause inflammation of the sinuses.
So, the next time you think about your bones, remember that they are not as solid as they might seem. They are actually quite complex structures that contain air-filled cavities that make them lighter and stronger. This is the magic of pneumatization!
Is pneumatization normal?
Think of it like this: Imagine your sinuses are like empty rooms in your skull. As you grow, these rooms gradually fill with air. This process is called pneumatization.
Why is this important? Well, pneumatization helps give our sinuses a few important jobs:
Lightening the skull: Imagine carrying around a heavy helmet all the time – that’s what your skull would be like without pneumatization.
Improving sound resonance: Ever notice how your voice sounds different when you have a stuffy nose? That’s because your sinuses help amplify sound.
Protecting your brain: Your sinuses act like a buffer zone, protecting your brain from injury.
It’s important to remember that pneumatization is a natural process that happens throughout our lives. If you have any concerns about your sinuses, it’s always best to talk to your doctor.
What is the role of mastoid Pneumatization in temporal bone fractures?
Mastoid pneumatization refers to the air-filled spaces within the mastoid bone. These spaces are connected to the middle ear and are lined with a thin layer of mucous membrane. This unique structure plays a key role in protecting the temporal bone from the forces of trauma.
Think of it like this: imagine a sponge. When you squeeze a sponge, the water inside it is forced out, absorbing the pressure and reducing the impact. The mastoid air cells function similarly. During a direct hit, the air within these cells helps to absorb the force of the blow. This helps to distribute the energy, preventing it from concentrating on a single point and potentially causing a fracture.
The degree of pneumatization can vary greatly from person to person. Some individuals have very well-developed mastoid air cells, while others have fewer and smaller cells. This difference in pneumatization can affect how the mastoid bone absorbs and disperses energy.
In individuals with well-developed mastoid air cells, the impact of trauma is distributed over a larger area, reducing the likelihood of fracture. On the other hand, individuals with poorly developed mastoid air cells may be more prone to fracture in the event of trauma, as the energy is concentrated in a smaller area.
Understanding the role of mastoid pneumatization is important for healthcare professionals who treat patients with temporal bone fractures. This knowledge can help them assess the severity of the injury and guide treatment decisions.
See more here: What Is The Theory Of Pneumatization Of The Mastoid? | Pneumatization Of Mastoid Air Cells Radiology
How symmetrical is the pneumatization of mastoid air cells?
Pneumatization is a process where air spaces develop within the bones of the skull. This process is particularly important in the temporal bone, which houses the ear and mastoid process. The mastoid process, a bony projection behind the ear, is filled with air cells that are connected to the middle ear cavity. The development of these air cells, called mastoid air cells, is a complex process that can vary significantly from person to person.
The symmetry of mastoid air cell pneumatization is important for several reasons. First, it helps to ensure that the air pressure within the middle ear is balanced, which is crucial for hearing. Second, the air cells provide a cushioning effect that protects the delicate structures of the inner ear from injury. Finally, the mastoid air cells play a role in the drainage of mucus from the middle ear.
While our study showed that mastoid air cell pneumatization is symmetrical in the majority of people, there can be significant variations between individuals. Some people may have more or fewer air cells, and the size and shape of the cells can also vary. These variations can be influenced by factors such as genetics, age, and environmental exposures.
It’s important to note that asymmetry in mastoid air cell pneumatization is not necessarily a cause for concern. However, if there is a significant asymmetry or if there are any other signs or symptoms of an ear problem, it is important to see a doctor for an evaluation.
What are mastoid air cells?
These air cells play a crucial role in making your temporal bone lighter and more resilient. They also help with sound transmission and, in a way, act as a buffer against infections. This is because air is a good insulator, preventing bacteria from easily spreading within the bone.
Let’s dive deeper into these fascinating structures:
Pneumatization: The Building Process
The development of mastoid air cells is called pneumatization. This process starts during childhood and continues into adulthood. During pneumatization, the bone around the middle ear gradually breaks down, creating these air-filled spaces. The process is influenced by factors like genetics and environmental conditions.
Variable Size and Extent
You might be wondering why the size and number of mastoid air cells vary. It’s because of the natural differences in our anatomy. Some individuals have extensive pneumatization, meaning their mastoid air cells are numerous and spread out. Others have limited pneumatization, with fewer and smaller cells.
Understanding the Implications
The size and extent of your mastoid air cells can have implications for your health, particularly in relation to ear infections. For example, individuals with extensive pneumatization might be more susceptible to certain types of ear infections because bacteria can travel more easily through the interconnected air cells. However, these cells can also offer a protective advantage by absorbing shock and reducing the impact of pressure changes within the ear.
In a nutshell, mastoid air cells are like tiny air pockets within your temporal bone. Their size and number vary, but they play an important role in making your bone lighter, absorbing shock, and potentially influencing the spread of ear infections.
Are mastoid air cells pneumatized?
Only a small percentage of patients, 8.7%, had diploic or poorly pneumatized mastoids. A sclerotic type was only seen in a single Indian patient, representing 0.7% of the study population.
What are pneumatized mastoid air cells?
The mastoid bone, located behind the ear, is a complex structure with numerous air-filled spaces called mastoid air cells. These cells are connected to the middle ear and are lined by a thin layer of mucous membrane. Pneumatization refers to the process of these air cells filling with air.
Why is it important to know if mastoid air cells are pneumatized?
The degree of pneumatization is important to understand for a few reasons:
Ear Infections:Pneumatized mastoid air cells can make it easier for infections to spread from the middle ear to the mastoid bone. This can lead to mastoiditis, a serious infection that can cause hearing loss and other complications.
Surgery: The degree of pneumatization can affect the planning and execution of ear surgery, such as tympanoplasty (ear drum repair) or mastoidectomy (surgery to remove parts of the mastoid bone).
Imaging:Pneumatization patterns can be seen on CT scans and X-rays, which helps doctors understand the anatomy of the middle ear and mastoid region.
How does pneumatization develop?
The development of mastoid air cells begins in early childhood and continues throughout adolescence. The degree of pneumatization varies depending on individual factors, such as genetics and environmental influences.
What are diploic and sclerotic mastoids?
Diploic mastoids have fewer air cells and more bone tissue. This can make them more susceptible to infection.
Sclerotic mastoids have dense bone tissue with very few air cells. This is less common and can make surgery more challenging.
Understanding the pneumatization status of mastoid air cells is crucial for the diagnosis and treatment of ear diseases.
Are mastoid air cells symmetrical?
Let’s break down what this means and why it’s important.
The mastoid air cells are a network of air-filled spaces within the mastoid bone, which is behind your ear. These cells can vary in size and shape from person to person, but they usually develop symmetrically, meaning that they’re similar on both sides of the head. The air cells help to lighten the skull, and they also play a role in sound transmission.
The sphenoid sinus, on the other hand, is a single air-filled space located in the middle of the skull, behind the nose. Like the mastoid air cells, the sphenoid sinus can vary in size and shape, and it also develops symmetrically.
Our research shows that there’s a link between the amount of air in the mastoid air cells and the sphenoid sinus. This suggests that these two areas of the skull develop together, and that changes in one area can affect the other.
While most people have symmetrical mastoid air cells, there are some cases where they’re not. This can happen for a number of reasons, such as:
Congenital malformations: Sometimes, people are born with mastoid air cells that are not symmetrical. This is usually due to a problem with the development of the skull during pregnancy.
Infection: Infection of the mastoid air cells (mastoiditis) can cause inflammation and swelling, which can lead to asymmetry.
Trauma: Injury to the skull, such as a fracture, can also damage the mastoid air cells and cause asymmetry.
If you have any concerns about the symmetry of your mastoid air cells, it’s important to talk to your doctor. They can examine you and determine if there’s any cause for concern.
See more new information: musicbykatie.com
Pneumatization Of Mastoid Air Cells Radiology | What Are Pneumatized Mastoid Air Cells?
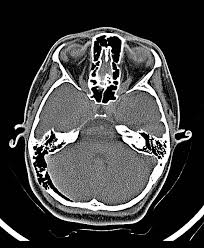
Alright, let’s talk about pneumatization of mastoid air cells, a topic that might sound a bit intimidating, but I promise it’s not that bad! Basically, it’s all about how air spaces in your skull develop, and how we can see them using radiology. This is important because the way these air cells look can tell us a lot about the health of your middle ear, inner ear, and even your temporal bone, which is the bone behind your ear.
So, picture this: your skull is like a big, complex house with lots of rooms, and some of those rooms are filled with air. These air-filled rooms are called mastoid air cells, and they start to develop during childhood. They are connected to the middle ear by a special passage called the Eustachian tube.
What’s the deal with pneumatization?
Pneumatization is the process of these air cells forming and growing. It’s like building new rooms in your skull house! This process can vary from person to person. Some people have very large and well-developed mastoid air cells, while others have smaller, less developed ones.
Radiology: The key to seeing inside the skull house
Now, radiology is our tool for peeking into these mastoid air cells. We use techniques like X-rays, CT scans, and MRI scans to get a good look inside. Each of these methods has its own strengths and weaknesses, and the choice depends on what we’re trying to find out.
X-rays are the simplest and most basic tool. They can show us the general shape and size of the mastoid air cells, but they don’t give us a lot of detail.
CT scans are like taking a 3D snapshot of your skull. They give us a much more detailed view of the mastoid air cells and surrounding structures.
MRI scans are best for looking at soft tissues. They can be helpful in seeing things like inflammation or tumors that might be affecting the mastoid air cells.
Why is this important?
Understanding how the mastoid air cells develop and look on these images can help us diagnose a whole range of conditions, including:
Otitis media: This is an inflammation of the middle ear, often caused by an infection.
Cholesteatoma: This is a benign but destructive growth that can form in the middle ear.
Mastoiditis: This is an infection of the mastoid air cells.
Facial nerve disorders: The facial nerve runs through the temporal bone, and problems with the mastoid air cells can sometimes affect this nerve.
Tumors: Tumors in the temporal bone can sometimes affect the mastoid air cells.
What are we looking for?
When we look at radiology images, we’re looking for things like:
Size and shape of the mastoid air cells: Are they large or small? Are they well-defined or poorly defined?
Presence of any abnormalities: This could include things like fluid, inflammation, tumors, or bone erosion.
Relationship to surrounding structures: Are the mastoid air cells close to important structures like the facial nerve or inner ear?
Understanding these things can help us figure out what’s going on and make a diagnosis.
Let’s talk about common variations in pneumatization
Here’s where it gets a bit more specific:
Sclerotic mastoid: This means the mastoid air cells are small and dense.
Pneumatized mastoid: This is the opposite; the mastoid air cells are large and well-developed.
Diploic mastoid: This is somewhere in between, with a mix of both small and large mastoid air cells.
It’s important to remember that these variations are normal and don’t always mean there’s a problem.
Keep in mind that pneumatization can also be affected by factors like:
Age: Mastoid air cells continue to develop throughout childhood.
Genetics: Some people are simply more likely to have larger mastoid air cells.
Previous ear infections: Inflammation from ear infections can affect the development of mastoid air cells.
Frequently Asked Questions (FAQs)
Q: Does the size of my mastoid air cells affect my hearing?
A: In most cases, no. The size of your mastoid air cells doesn’t usually affect your hearing. However, if there’s a problem with the middle ear or inner ear that’s affecting your hearing, the size of the mastoid air cells might be a factor.
Q: Can I do anything to make my mastoid air cells bigger?
A: Not really. The size of your mastoid air cells is mostly determined by genetics and your development.
Q: Should I be worried if my mastoid air cells look different on a scan?
A: Don’t panic! Variations in the size and shape of the mastoid air cells are common, and they don’t always mean there’s a problem. Your doctor will be able to tell you if anything needs to be addressed.
Q: How can I learn more about this?
A: You can always talk to your doctor or an audiologist. There are also a lot of reliable resources online, like medical journals and patient information websites.
In conclusion, understanding pneumatization of mastoid air cells is a key part of diagnosing and treating conditions affecting the ear, temporal bone, and surrounding structures. While it might sound complicated, with the help of radiology, we can get a clear picture of what’s going on inside your skull! Just remember, if you have any concerns, always talk to your doctor.
Hyperpneumatisation of mastoid air cells | Radiology Case
Excessive pneumatization of the mastoid air cells extending along occipital bone including condyle, clivus, and right petrous apex. Loculated and septated air collection Radiopaedia
Hypopneumatisation of the mastoid air cells | Radiology Case …
Hypopneumatisation of the mastoid air cells is typically an anatomical variant. There may or may not be a link to otitis media with effusions in childhood. Radiopaedia
Pneumatization of the Mastoid | Radiology – RSNA Publications
THIS communication purposes to trace the growth and development of the mastoid radiographically; to correlate roentgen findings to anatomic and clinical conceptions, RSNA Publications Online
Temporal bone pneumatization: A scoping review on the growth
Mastoid air cells in females was larger and increased significantly. However, among Bangele people of Indian, mastoid air cells increase by about 2 cm 2 every 5 National Center for Biotechnology Information
Pneumatization Pattern and Status of the Mastoid Antrum in
Epithelium infiltrates the growing bone and produces epithelium-lined air cell chambers, a process known as pneumatization. Conventional temporal bone National Center for Biotechnology Information
Pneumatization of Mastoid Air Cells, Temporal Bone, Ethmoid
The PNS and other parts of temporal bone like mastoid air cells system have been found to have multiple functions including humidification, adding resonance National Center for Biotechnology Information
Classification of mastoid air cells by CT scan images using deep …
In general, the mastoid air cells are either pneumatized or none pneumatized. in the case of none pneumatization, it could have either opacification or Journal of Big Data
Imaging Review of the Temporal Bone: Part I.
From a clinical-radiologic standpoint, there are a limited number of structures and disease entities in the temporal bone with which one must be familiar in order to proficiently interpret a computed RSNA Publications Online
Pneumatization of Mastoid Air Cells, Temporal Bone, Ethmoid
The aim of this study is to assess the pneumatization of the paranasal sinuses (PNS) and other parts of temporal bone such as mastoid air cells and to investigate if there was PubMed
Case 602 Enlarged Normal Mastoid Bone
Mastoid Air Cells And Mastoid Pneumatization.Mp4
Temporal Bone Anatomy
Temporalbone And Sphenoid Pneumatization
Mastoiditis Causing Csvt Bilateral Transverse And Superior Sagittal Sinus Thrombosis
Computed Tomography (Ct) Of The Paranasal Sinuses+Mastoid Air Cells
Radiology Of Cochlear Implant ( Video 4 )
Otology | Ct Temporal Bone: ‘What The Surgeons Want To Know’ | Panel Discussion
Link to this article: pneumatization of mastoid air cells radiology.
See more articles in the same category here: https://musicbykatie.com/wiki-how/
